تأثیر بسته ی تحرکی بر پنومونی مرتبط با مراقبت های بهداشتی غیر ونتیلاتور (NV-HAP) در بیماران بستری در بیمارستان: یک مرور نظام مند
کد: G-1129
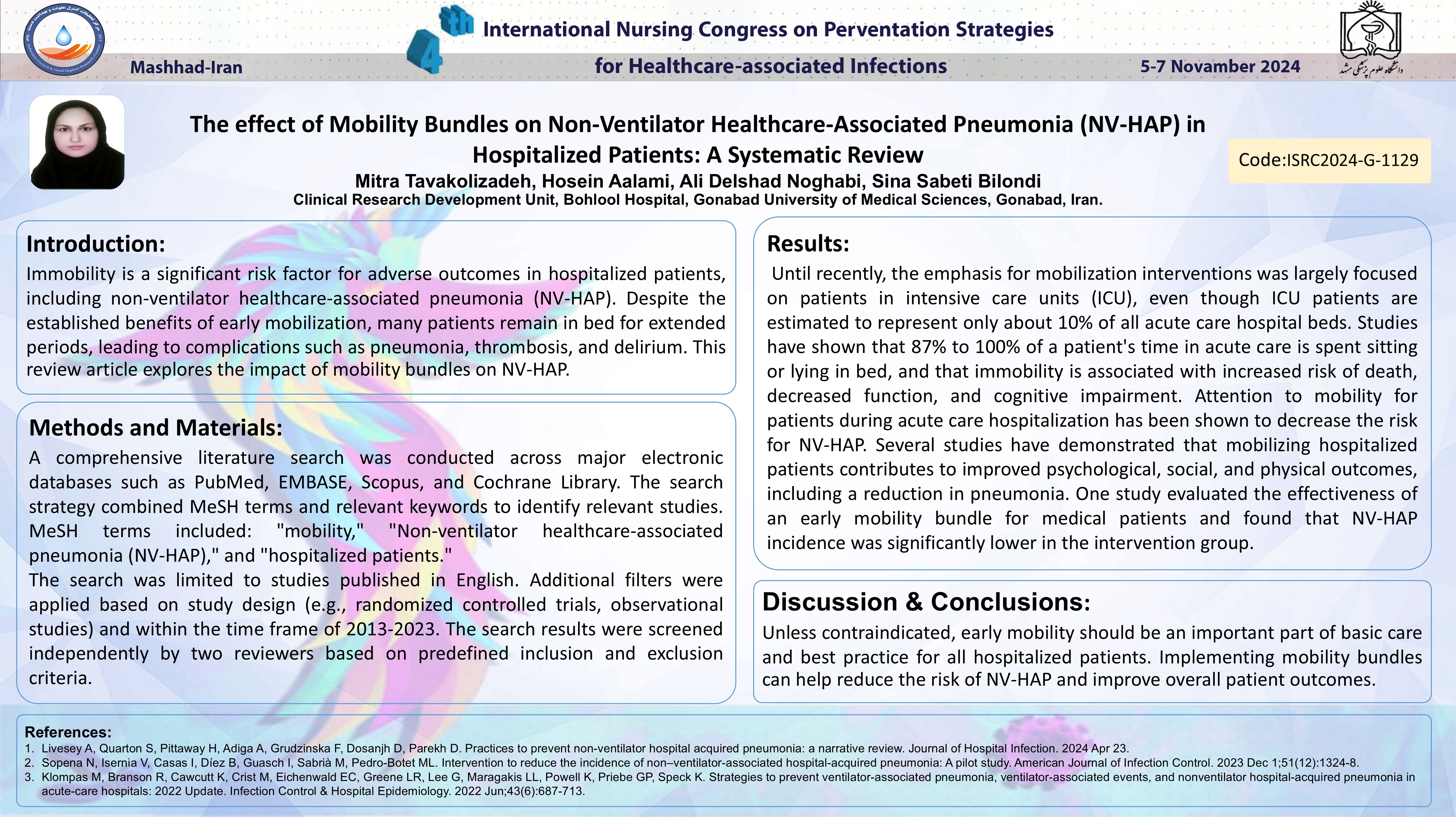
نویسندگان: Mitra Tavakolizadeh © ℗, Hosein Aalami, Ali Delshad, Sina Sabeti Bilondi
زمان بندی: زمان بندی نشده!
دانلود: دانلود پوستر
خلاصه مقاله:
خلاصه مقاله
Introduction: Immobility is a significant risk factor for adverse outcomes in hospitalized patients, including non-ventilator healthcare-associated pneumonia (NV-HAP). Despite the established benefits of early mobilization, many patients remain in bed for extended periods, leading to complications such as pneumonia, thrombosis, and delirium. This review article explores the impact of mobility bundles on NV-HAP. Search Strategy: A comprehensive literature search was conducted across major electronic databases such as PubMed, EMBASE, Scopus, and Cochrane Library. The search strategy combined MeSH terms and relevant keywords to identify relevant studies. MeSH terms included: "mobility," "Non-ventilator healthcare-associated pneumonia (NV-HAP)," and "hospitalized patients." The search was limited to studies published in English. Additional filters were applied based on study design (e.g., randomized controlled trials, observational studies) and within the time frame of 2013-2023. The search results were screened independently by two reviewers based on predefined inclusion and exclusion criteria. Results: Until recently, the emphasis for mobilization interventions was largely focused on patients in intensive care units (ICU), even though ICU patients are estimated to represent only about 10% of all acute care hospital beds. Studies have shown that 87% to 100% of a patient's time in acute care is spent sitting or lying in bed, and that immobility is associated with increased risk of death, decreased function, and cognitive impairment. Attention to mobility for patients during acute care hospitalization has been shown to decrease the risk for NV-HAP. Several studies have demonstrated that mobilizing hospitalized patients contributes to improved psychological, social, and physical outcomes, including a reduction in pneumonia. One study evaluated the effectiveness of an early mobility bundle for medical patients and found that NV-HAP incidence was significantly lower in the intervention group. Conclusion: Unless contraindicated, early mobility should be an important part of basic care and best practice for all hospitalized patients. Implementing mobility bundles can help reduce the risk of NV-HAP and improve overall patient outcomes.
کلمات کلیدی
mobility bundle, Non-ventilator healthcare-associated pneumonia (NV-HAP), hospitalized patients, systematic review